Researchers at the Centre for Genomic Regulation (CRG) have developed the first experimental “living medicine” to treat antibiotic-resistant bacteria that grow on the surfaces of medical implants, reports Science Daily. Infections that affect medical implants are often resistant to antibiotic treatment and account for 80% of all hospital acquired infections. The surfaces of medical implants also provide “ideal growing conditions for biofilms” where “biofilm-associated bacteria can be a thousand times more resistant to antibiotics than free-floating bacteria.”
Biofilm infections that cannot be treated with conventional antibiotics often require an additional surgical procedure to remove the infected hardware. Alternative treatments include the broad-spectrum use of antibodies or enzymes, which are highly toxic to normal tissues and cells. The authors of this study thus hypothesized that the safest and most cost-effective way of targeting biofilms was to introduce living organisms that produce enzymes in the local area of surrounding biofilms. Researchers selected to engineer Mycoplasma pneumoniae bacteria as a vector for this study because it lacks a cell wall, “making it easier to release the therapeutic molecules that fight infection while also assisting it in evading detection from the human immune system.”
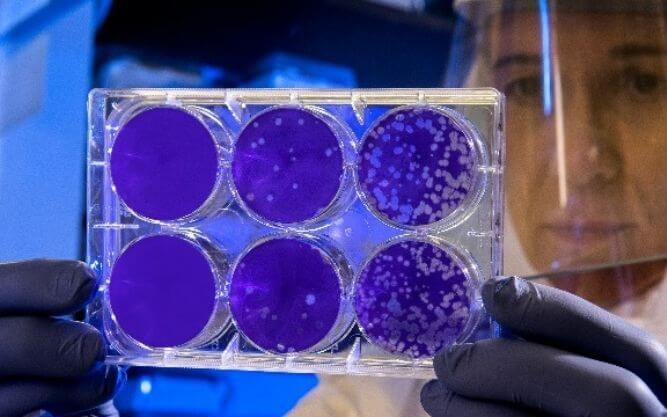
M. pneumoniae cells were modified to produce enzymes that break down biofilms and attack the cell walls of embedded bacteria, and to secrete antimicrobial enzymes more effectively. Because M. pneumoniae are naturally adapted to the lung environment, researchers aim to first use this therapy to treat biofilms forming around breathing tubes. Maria Lluch, co-corresponding author of the study, assures that this technology has been “designed to meet all safety and efficacy standards for application in the lung,” and addressed the need to tackle the challenge of high-scale production and manufacturing that is required to begin clinical trials in 2023.
Luis Serrano, Research Professor and Director of the CRG, believes that the use of genetically modified bacteria as a “living medicine” will have vast applications because “they can carry any given therapeutic protein to treat the source of a disease.” Future applications could include the treatment of biofilms on catheters, pacemakers, and prosthetic joints.